Knee osteoarthritis (OA) can be characterised as non-traumatic or post-traumatic. Whereas, non-traumatic OA occurs without any history of acute knee injury, post-traumatic OA, as the name implies, develops following knee trauma.
1. Knee osteoarthritis often develops in adolescence and young adulthood, prior to 40 years of age:
The most striking and important difference of post-traumatic knee OA, is its early-onset compared to non-traumatic OA. Approximately 50% of people who suffer an anterior cruciate ligament (ACL) or meniscal tear will have radiographic (X-ray) OA within a decade. As these injuries typically occur in active adolescents and young adults, knee OA develops prior to 40 years of age, which is much earlier than the general population without knee injury. Unlike older adults with OA, these young adults typically have high physical demands (e.g. occupational, parental, sporting), which is important to consider when discussing goals and planning clinical management.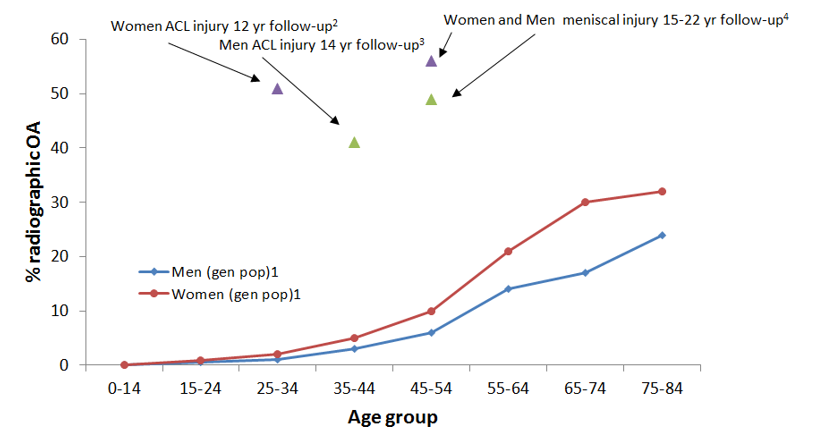
- Australian Institute of Health & Welfare: 2004-2005 National Health Survey
- Von Porat ARD 2004; 3. Lohmander A&R 2004; 4. Englund A&R 2003
2. In post-traumatic osteoarthritis, structural changes are more likely in the lateral compartments:
In older people with non-traumatic osteoarthritis, structural joint changes, such as osteophyte growth (bony spurs) and joint space narrowing (bone-to bone), predominantly  occur to the medial compartment. However, in post-traumatic osteoarthritis, structural changes are more evenly distributed between the medial and lateral compartments (Swärd et al., 2010). This is likely due to the more common lateral compartment damage inflicted at the time of knee trauma, and altered biomechanics following injury (Stein et al., 2012). Treatments that focus on the medial compartment, such as knee braces to unload the medial part of the joint, may not be as effective in post-traumatic OA.
occur to the medial compartment. However, in post-traumatic osteoarthritis, structural changes are more evenly distributed between the medial and lateral compartments (Swärd et al., 2010). This is likely due to the more common lateral compartment damage inflicted at the time of knee trauma, and altered biomechanics following injury (Stein et al., 2012). Treatments that focus on the medial compartment, such as knee braces to unload the medial part of the joint, may not be as effective in post-traumatic OA.
3. People with post-traumatic knee OA walk with different biomechanics compared to people with non-traumatic OA:
Specifically, people with post-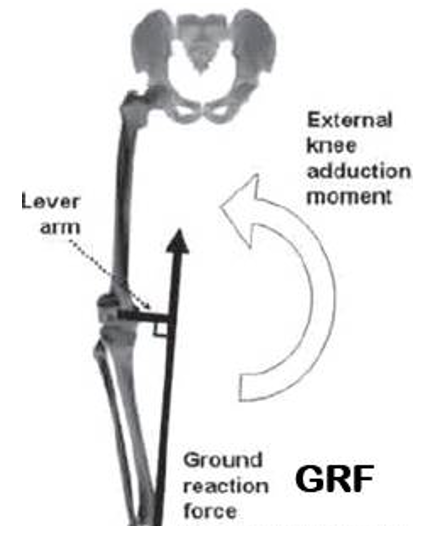 traumatic OA display lower knee adduction angles (less bow legged) and lower knee adduction moments (less loading of medial compartment) than non-traumatic OA (Robbins et al., 2016). Post-traumatic OA is thought to be more strongly driven instead by external rotation differences (greater knee roll out) during walking and running, as this is a common feature of ACL injured and reconstructed knees (Scanlan et al., 2010). Braces, footwear or gait retraining programs designed to reduce the knee adduction moment may not be appropriate for patients with post-traumatic knee OA, but instead may need to focus on reducing excessive external rotation.
traumatic OA display lower knee adduction angles (less bow legged) and lower knee adduction moments (less loading of medial compartment) than non-traumatic OA (Robbins et al., 2016). Post-traumatic OA is thought to be more strongly driven instead by external rotation differences (greater knee roll out) during walking and running, as this is a common feature of ACL injured and reconstructed knees (Scanlan et al., 2010). Braces, footwear or gait retraining programs designed to reduce the knee adduction moment may not be appropriate for patients with post-traumatic knee OA, but instead may need to focus on reducing excessive external rotation.
4. Cartilage deterioration can be caused by changes in joint fluid:
Compared to non-traumatic OA, post-traumatic OA is associated with decreased joint fluid viscosity (thickness) and increased activity from a joint fluid antioxidant enzyme, which may contribute to cartilage deterioration (Ostalowska et al., 2006). As joint fluid covers the whole joint, this may contribute to a high prevalence of lateral compartment and patellofemoral (kneecap) joint OA following knee trauma (Culvenor et al., 2013). Don’t forget the patellofemoral joint – a distinct entity requiring its own management approach!
Don’t assume that people with post-traumatic knee OA have the same characteristics as those with non-traumatic knee OA. Clinical management needs to be individualised to specific impairments in each case, and to each patient’s unique needs and goals.