We know that development of osteoarthritis (OA) after ACL reconstruction occurs in over 50% of patients. The question is, should we inform our patients of this, and if so how should we go about this. Anecdotally, consensus is that this can be a tricky conversation, and something that may be avoided by some therapists due to fear of alarming the patient.
What is current state of patient knowledge?
- 65% thought ACLR reduced their risk of OA or did not know.
- Only 26% had a discussion with their therapist regarding OA. Bennell et al., (2016)
Key discussion points for ACLR patients:
- ACLR patients may not be symptomatic in early years post surgery, but there is a possibility of future symptoms and joint pathology and this is normal.
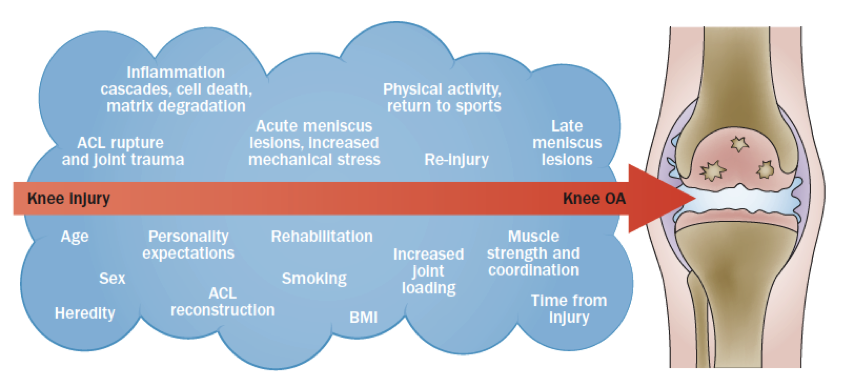
- The development of symptoms or joint changes is due to the interaction of many factors. This great graphic by Wen and Lohmander (2014) can help explain these:
- Communicating the importance of achieving optimal strength and function, goal based return to activity, maintenance of neuromuscular exercises may help. This may reduce joint loads, risk of re injury and symptomatic decline.
Will my ACLR patient catastrophise after an imminent diagnosis of OA?
There is no research analysing behaviour/intervention change in ACLR population. However, a study by Grindrod et al., 2010 in a group of 50 year old people with early signs of OA showed that after an official “diagnosis of OA” and administration of a self management program, they implement the following:
- Increase in medications and supplements
- Increased use of NSAIDs to self-manage pain
- Increase in exercise interventions
Overall patients were pro-active in doing something about their condition, and this actually resulted in increased self reported function and quality of life. However the decisions about type of medication and exercise were made independently, and not always guided by professionals. Therefore, although self management is important, this management must initially be guided by professionals and communicated clearly to patients.
What is the benefit of informing the patient about their risk of OA?
The potential importance of early intervention
We do not know whether the rate of OA progression can be altered by therapeutic interventions. However, we have some evidence to suggest better long-term outcomes post ACL reconstruction is related to those who have better strength, function and biomechanics. This may aid in motivation to ensure deficits are addressed completely and more importantly continue to maintain their strength and function (i.e. conservative management of OA) in to the future.
Matching of expectations
Awareness of potential lifestyle modifications that may have to occur may improve patient satisfication. Filbay et al., (2016) demonstrated those who adapt their lifestyle after ACL reconstruction to accommodate knee impairments is associated with greater acceptance and satisfaction, irrespective of knee symptoms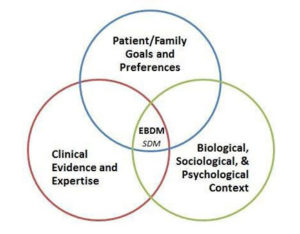
Shared decision making
A great editorial recently highlighted the important of “shared decision making” in treatment of patellofemoral pain.
In respect to ACLR patients, sharing knowledge with patients about expected outcomes, how this relates to return to sport timing, types of activity they may participate in the future will aid in satisfication and quality of life.