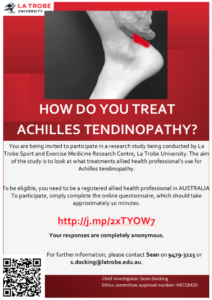
If you are an allied health professional in Australia, can you please spare 5-10 minutes and help us out. We’d love you to complete a short survey on how you treat Achilles tendinopathy. Link: http://j.mp/2xTYOW7
This is the saddest time in my yearly academic cycle. It is the day that is the furthest away from the next International Scientific Tendinopathy Symposium. The event where the biggest tendon nerds and ‘tendoholics’ gather to discuss tendons. All I can do to make myself feel better is write about some highlights from the conference.
Firstly, a big thank you and congratulations to Prof Hans Zwerver and the scientific committee on the success of the conference. As you can imagine, it was extremely well organised and the new innovations as part of the conference were fantastic.
- In tendons, like chocolate lava cakes, we need to get excited by the ‘gooey’ bit.
 Rather than delicious molten chocolate, Prof Hazel Screen was referring to the interfascicular matrix (IFM). The IFM has lots of lubricin (no extra points for figuring out its role) and a large number of metabolically active cells. While our tendons are predominately collagen, “collagen does very little and is pretty inert”. The majority of tendons springy behaviour comes from inter-fascicular slide and glide. The sad news is that you lose your IFM with age and mechanical loading, resulting in a tendon that isn’t ideally suited to energy-storage. The obvious question is how do we maintain our IFM through age and can that reduce our risk of injury? Also, where can I get a chocolate lava cake.
Rather than delicious molten chocolate, Prof Hazel Screen was referring to the interfascicular matrix (IFM). The IFM has lots of lubricin (no extra points for figuring out its role) and a large number of metabolically active cells. While our tendons are predominately collagen, “collagen does very little and is pretty inert”. The majority of tendons springy behaviour comes from inter-fascicular slide and glide. The sad news is that you lose your IFM with age and mechanical loading, resulting in a tendon that isn’t ideally suited to energy-storage. The obvious question is how do we maintain our IFM through age and can that reduce our risk of injury? Also, where can I get a chocolate lava cake. - Tendon pain is a pain!!! Compared to previous ISTS meetings, there has certainly been an increased focus and appreciation of the features of tendon pain and how we may address them. Dr Ebonie Rio laid down the challenge for us to become amazing bioplasticians in treating tendon pain. The body is incredibly adaptable; it will find
 ways to adapted to continue to function, and we can use that plasticity to expose it to therapies to redress these potential maladaptations in tendon tendon, muscle, and motor cortex. Our understanding is certainly improving around pain, with Melanie Plinsinga and Henrik Riel showing sensory alterations in people with gluteal tendinopathy and plantar heel pain, respectively. But there is a person attached to those sensory changes, an avoidance of physical activity and decreased quality of life. We are beginning to appreciate the biopsychosocial model of pain in the treatment of tendons. You need to address and discuss their pain, all with the aim of improving patients’ self-efficacy to complete their exercises and address the bio component of the model.
ways to adapted to continue to function, and we can use that plasticity to expose it to therapies to redress these potential maladaptations in tendon tendon, muscle, and motor cortex. Our understanding is certainly improving around pain, with Melanie Plinsinga and Henrik Riel showing sensory alterations in people with gluteal tendinopathy and plantar heel pain, respectively. But there is a person attached to those sensory changes, an avoidance of physical activity and decreased quality of life. We are beginning to appreciate the biopsychosocial model of pain in the treatment of tendons. You need to address and discuss their pain, all with the aim of improving patients’ self-efficacy to complete their exercises and address the bio component of the model. - Look deep inside my tendon and tell me what’s wrong. As always, there was a strong imaging presence at ISTS, with radiologist Assoc Prof Edwin Oei providing the keynote. Imaging can be separated into two categories; a “tool” to help us understand the biology of tendons, and as a clinical “biomarker” where we use imaging to diagnose and direct treatments. As far as imaging as a “tool”, multiple research groups using everything from UTC to shear-wave elastography, showed that imaging can detect responses to load. Great as a research tool, but the jury is still out for imaging as a clinical “biomarker”. Dr Lorenzo Masci showed that UTC had limitations as a predictive tool for the development of Achilles tendinopathy in 223 rugby players (a study with that many scans is probably predictive of repetitive strain disorder. Huge effort by Lorenzo). Axial shearwave wasn’t much better, with its ability to diagnose pain questionable (may be an understatement with Assoc Prof Preston Wiley showing a specificity of 19%!!). Hopefully, with the formation of a working group for a consensus on imaging we may be able to bring some clarity.
- When will he talk about how we treat tendinopathy!!!! The debate rages on about what is the most effective loading intervention. We still have a long way to go but at least we have options for different individuals and different situations. Ch
 ris Clifford from Glasgow found that both isometrics and isotonics were effective at reducing pain in gluteal tendinopathy. For lateral elbow tendinopathy, isometrics improved pain in comparison to wait-and-see. A little tip from Viana Vuvan was that if it took longer that 5-10mins to settle following isometrics in the first week, they were likely to have a poor outcome at 12 weeks. Assoc Prof Peter Malliaras and team found isometrics immediately reduced hop pain in midportion Achilles tendinopathy. Finally, Heinrik Riel found no difference in isometrics, isotonics, or walking for immediate changes in pain in plantar fasciopathy. The good news is that there are still long-term benefits for pain in performing high-load strength training in these patients. There is one thing for sure, we are no closer to having THE answer but overwhelmingly we are seeing that some form of a loading intervention is our best bet for people with tendinopathy
ris Clifford from Glasgow found that both isometrics and isotonics were effective at reducing pain in gluteal tendinopathy. For lateral elbow tendinopathy, isometrics improved pain in comparison to wait-and-see. A little tip from Viana Vuvan was that if it took longer that 5-10mins to settle following isometrics in the first week, they were likely to have a poor outcome at 12 weeks. Assoc Prof Peter Malliaras and team found isometrics immediately reduced hop pain in midportion Achilles tendinopathy. Finally, Heinrik Riel found no difference in isometrics, isotonics, or walking for immediate changes in pain in plantar fasciopathy. The good news is that there are still long-term benefits for pain in performing high-load strength training in these patients. There is one thing for sure, we are no closer to having THE answer but overwhelmingly we are seeing that some form of a loading intervention is our best bet for people with tendinopathy
Other little gems
-Paul Kirwan used his mnemonic device ‘Screen ‘Em’ to make sure we pick up inflammatory arthritis in those who present with tendinopathy so you can quickly refer on patients to get appropriate treatment.
-It’s questionable how much the high volume part of high volume injection is responsible for clinical outcomes in the Achilles. Peter Malliaras presented data to suggest that any improvement in pain was due to the corticosteroid that is used in combination with HVI.
-Keep an eye out for the upcoming consensus documents. A great initiative by the committee to make sure we have consensus on core domains for outcome measures, terminology, and minimum reporting for studies in tendinopathy.
Well done to all involved.
Dr Sean Docking