Part 2 of this blog continues on with the summary of @STSkou’s paper related to exercise and physical activity for osteoarthritis.
Just as other pain killers, exercise therapy needs to be taken at a sufficient dose and duration to ensure an optimal and clinically-relevant effect on pain and functional limitations.
 There is no universal exercise therapy program that will give all people with hip and knee OA the same clinical effect. Instead the program needs to be individualized based on patient characteristics to improve outcomes further, e.g. a previous study suggests that people with a varus thrust would improve more in pain from neuromuscular exercise therapy, while obese people would improve more in pain from quadriceps strengthening exercise therapy.
There is no universal exercise therapy program that will give all people with hip and knee OA the same clinical effect. Instead the program needs to be individualized based on patient characteristics to improve outcomes further, e.g. a previous study suggests that people with a varus thrust would improve more in pain from neuromuscular exercise therapy, while obese people would improve more in pain from quadriceps strengthening exercise therapy.
Starting with at least 12 supervised exercise therapy sessions of 30-60 minute duration seems to be important for the clinical effect, while extending the program to adhere to the exercise prescription recommendations for adults from the American College of Sports Medicine has the potential to improve the outcome further. The exercise therapy should preferably be supported by patient education to guide patients in the management of their own disease and ensure long-term motivation and adherence; a key parameter to sustain long-term effects. To reassure the patient it is important to highlight that the radiographic severity and baseline pain is not associated with the improvements in pain that the patient can expect following exercise therapy.
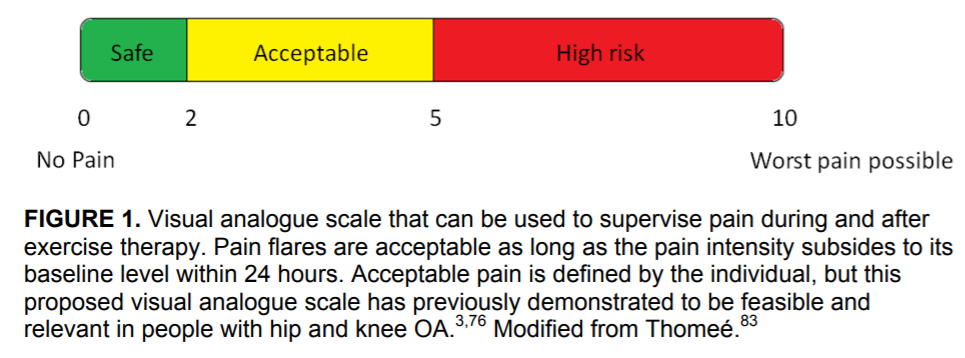
Pain during exercise is allowed and exercise-induced pain flares are common in the first few weeks of an exercise therapy program, but they will decrease over time. A rule of thumb that is safe to apply in clinical practice, is that if the patient finds the pain during exercise to be acceptable and if any increase in pain and symptoms during the exercise is reduced to the pre-exercise level within 24 hours the level of difficulty of the exercises is not too high.
WHERE TO NEXT?
As presented the evidence supporting the effects of exercise therapy in hip and knee OA and other chronic condition is substantial, underlining that it should be part of first line treatment. However, as implementation in clinical practice is suboptimal one of the most important future agendas is implementation of evidence.
Good Life with osteoarthritis from Denmark (GLA:D) represents one initiative aimed at improving the quality of care in clinical practice. GLA:D consists of two sessions of patient education and 12 sessions of supervised, individualized neuromuscular exercise therapy delivered by trained health care practitioners and evaluated in a national clinical registry. The program has been implemented in Denmark and is currently being implemented in Canada, Australia and China.
Listen to the podcast by Dr. Søren Thorgaard Skou talking about the GLA:D Program for Osteoarthritis:
Below are some videos demonstrating some exercises from GLA:D: